Modulating the CBD/Apelinergic System Interaction as a COVID-19 Treatment?
Although CBD has long been implicated as an anti-inflammatory agent, it is only within the past few decades that it has gained experimental evidence in support of such effects.
Notably, previous work published in Cannabis and Cannabinoid Research uncovered a potential role for CBD in ameliorating clinical symptoms of acute respiratory distress syndrome (ARDS) via cytokine storm regulation.
In extreme cases of respiratory viral infection – such as in severe cases of COVID-19 – massive pulmonary inflammation and enhanced inflammatory responses within the bronchoalveolar units of lower respiratory tracks result in a cytokine storm that leads to ARDS development.
In this initial study, a murine model of ARDS was developed and then used to investigate whether CBD treatment was able to alleviate ARDS-like symptoms associated with COVID-19 (including “low oxygen saturation, lymphopenia, elevated frequencies of neutrophils/monocytes, excess production of pro-inflammatory cytokines, and destruction of lung morphology”) following simulated viral infection with synthetic RNA.
Based on the results of this preliminary study – using the aforementioned murine ARDS model – the researchers sought to delve further into interrogating the therapeutic potential of CBD in the context of viral respiratory infections.
Published in the Journal of Cellular and Molecular Medicine, their follow-up study interrogated the mechanism responsible for modulating CBD’s previously observed anti-viral properties. ARDS-like symptoms were induced via simulated viral infection with a synthetic double-stranded RNA (dsRNA) analog, polyinosinic:polycytidylic acid (Poly(I:C)).
12-week-old adult male C57B1 mice randomly split into three experimental groups (n = 10 mice/group) received either one of the following treatments (once daily intranasal administration over three days): Group 1 = sterile saline [control]; Group 2 = Poly(I:C) [emulates ARDS]; and Group 3 = Poly(I:C) but also received additional intraperitoneal CBD treatment (3 doses total administered at designated time-points).
At the study’s onset and throughout its duration, researchers measured blood oxygen saturation in the carotid arteries of all mice with a portable pulse oximeter. Blood and lung tissue that were harvested following sacrifice underwent flow cytometry, immunofluorescence (IF), and histological analyses (fluorescence imaging, bright field microscopy, and Masson’s Trichrome staining of collagen fibers on fixed lung tissue sections).
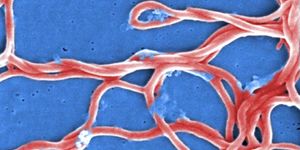
Whole blood and lung tissues from Poly(I:C)-treated mice demonstrated pathologic features of ARDS as well as marked reductions in apelin expression relative to the controls. The additional CBD treatment in Group 3 mice appeared to alleviate ARDS symptoms by restoring inflammatory homeostasis (increased T cells / decreased neutrophils, perivascular and peri-bronchiolar histopathological changes). Notably, CBD treatment also increased apelin expression in Group 3 mice towards levels comparable to the controls.
Apelin is an endogenous ligand that also acts as a second catalytic substrate for the receptor recognized by the SARS-CoV2 spike protein, the angiotensin-converting enzyme 2 (ACE2) receptor. It is also a ligand for APJ (a G protein-coupled receptor) – an interaction collectively referred to as the apelinergic system.
From these results, the authors concluded that a potential interaction between the apelinergic system and CBD is likely responsible for CBD’s observed anti-inflammatory effects. This most recent study, along with their previous work, provide encouraging evidence that modulating this interaction harbors the potential to improve COVID-19 patient outcomes.
Sources: Cannabis and Cannabinoid Research; NIH National Cancer Institute; Journal of Cellular and Molecular Medicine; Annals of the New York Academy of Sciences