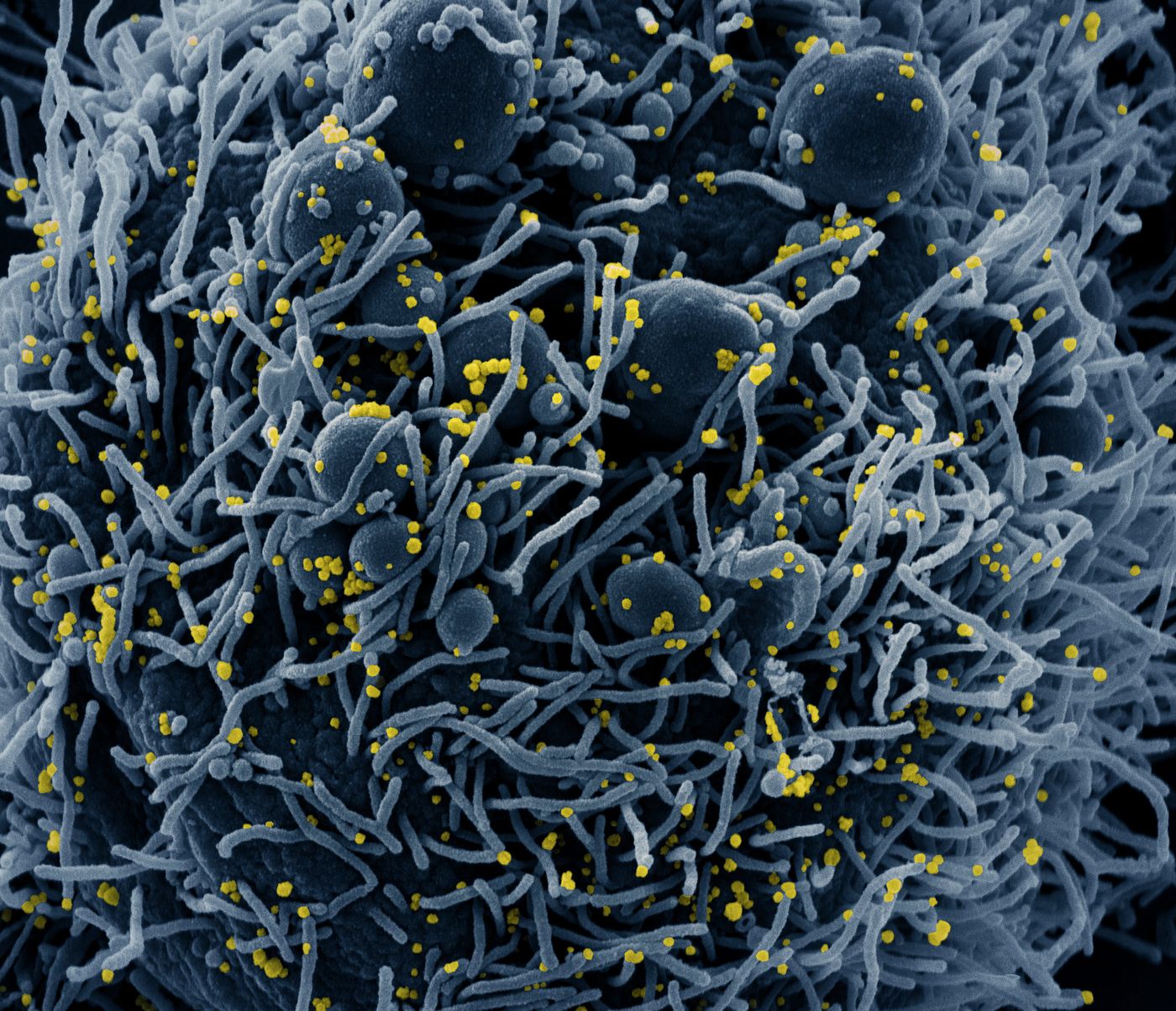
Mild COVID-19 Cases Induce an Immune Cell Response
As the pandemic virus, SARS-CoV-2 continues to cause tens of thousands of new cases of COVID-19 every day in the United States, and many more around the world, scientists are starting to learn more about the infection. One big question has been whether people that are infected with the virus become immune to reinfection. There are, after all, some viruses that can get worse on re-exposure, like dengue. It seems that in the cases of SARS-CoV-2, however, there is evidence that even very mild cases of COVID-19 result in a robust response in which memory T cells are activated, even when antibodies specific to the virus cannot be detected.
The findings, which have been reported in Cell, could be great news, and certainly reinforces the idea that a safe, effective vaccine might help bring the pandemic to an end. There have been a few cases in which patients that have recovered from COVID-19 seem to have recovered fully and then been reinfected at a later time. Right now, that doesn't seem to be happening outside of a few instances. The study authors suggested that recurrent episodes of severe COVID-19 might be prevented by the memory T cells that are triggered by the virus (and would act as the body's 'memory' of the infection so upon re-exposure, the body would fight it off more effectively).
"We are currently facing the biggest global health emergency in decades," said the senior study author Marcus Buggert of the Karolinska Institutet. "In the absence of a protective vaccine, it is critical to determine if exposed or infected people, especially those with asymptomatic or very mild forms of the disease who likely act inadvertently as the major transmitters, develop robust adaptive immune responses against SARS-CoV-2."
So far, most work that has investigated whether there is immunity to the pandemic virus after an infection has been focused on the detectable presence of antibodies that are neutralizing - they can bind to the virus and stop it from infecting cells. But antibodies won't be detectable in all people even when there is protection. Antibody levels can wane, especially in people with less severe cases.
A mouse model of the SARS-CoV-1 virus, which caused SARS, showed that memory T cells produced by exposure to a vaccine persisted for years, even when antibodies could not be identified.
In this study, the researchers looked at people in Sweden that represented a spectrum of COVID-19 cases. T cell responses were linked to how severe the disease was.. Memory T cells that were specific for SARS-CoV-2 were identified after the patients recovered, and the most severe cases had the strongest T cell response, while mild cases had a more limited response.
The scientists also found that family members who had been exposed to people with COVID-19 also had memory T cell responses that were specific to SARS-CoV-2. Of 28 family members that were exposed, 17 had antibody responses, and 26 had T cell responses.
"Our findings suggest that the reliance on antibody responses may underestimate the extent of population-level immunity against SARS-CoV-2," Buggert said. "The obvious next step is to determine whether robust memory T cell responses in the absence of detectable antibodies can protect against COVID-19 in the long-term."
It's also worth noting that this was not a study in which the individuals were deliberately exposed to SARS-CoV-2 to assess how well the T cells protected them. The scientists also wrote that severe re-infections were likely to be prevented, not that there wouldn't be a second infection. This work also does not show that herd immunity is a way out of our current crisis. Estimates have suggested that more than 70% of the population would have to be infected before that would be achieved, causing millions of deaths and likely overwhelming the health care system.
Sources: AAAS/Eurekalert! via Cell Press, Cell