How Rare Intestinal Cells May Work as a Kind of Therapeutic Sensor
The trillions of microbes in our gastrointestinal tract, known as the gut microbiome, are crucial to the body; the gut microbiome aids in digestion, nutrient absorption, and influences our health in different ways. But the body also has to be protected from all of those microbes, which are kept behind a tight barrier. But if the intestinal barrier is dysfunctional, or leaky, serious problems can arise.
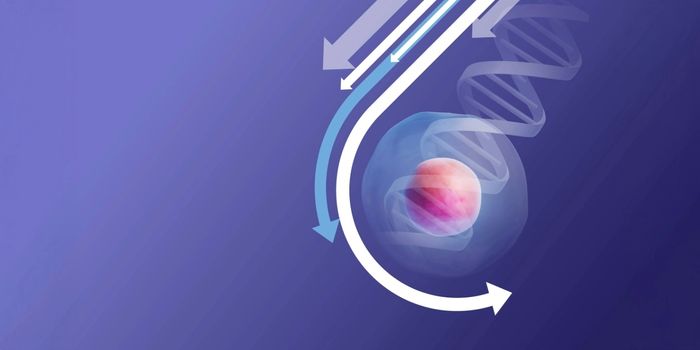
There are cells in the gut called enteroendocrine cells (EECs) that can generate hormones, which may have a variety of effects on the body. EECs release hormones in response to cues like food intake and stomach stretching. The hormones can then influence physiological processes related to digestion or appetite. Scientists have now found receptors on EECs that control hormone release. It may one day be possible to alter these receptors to treat disease. The research has been reported in Science.
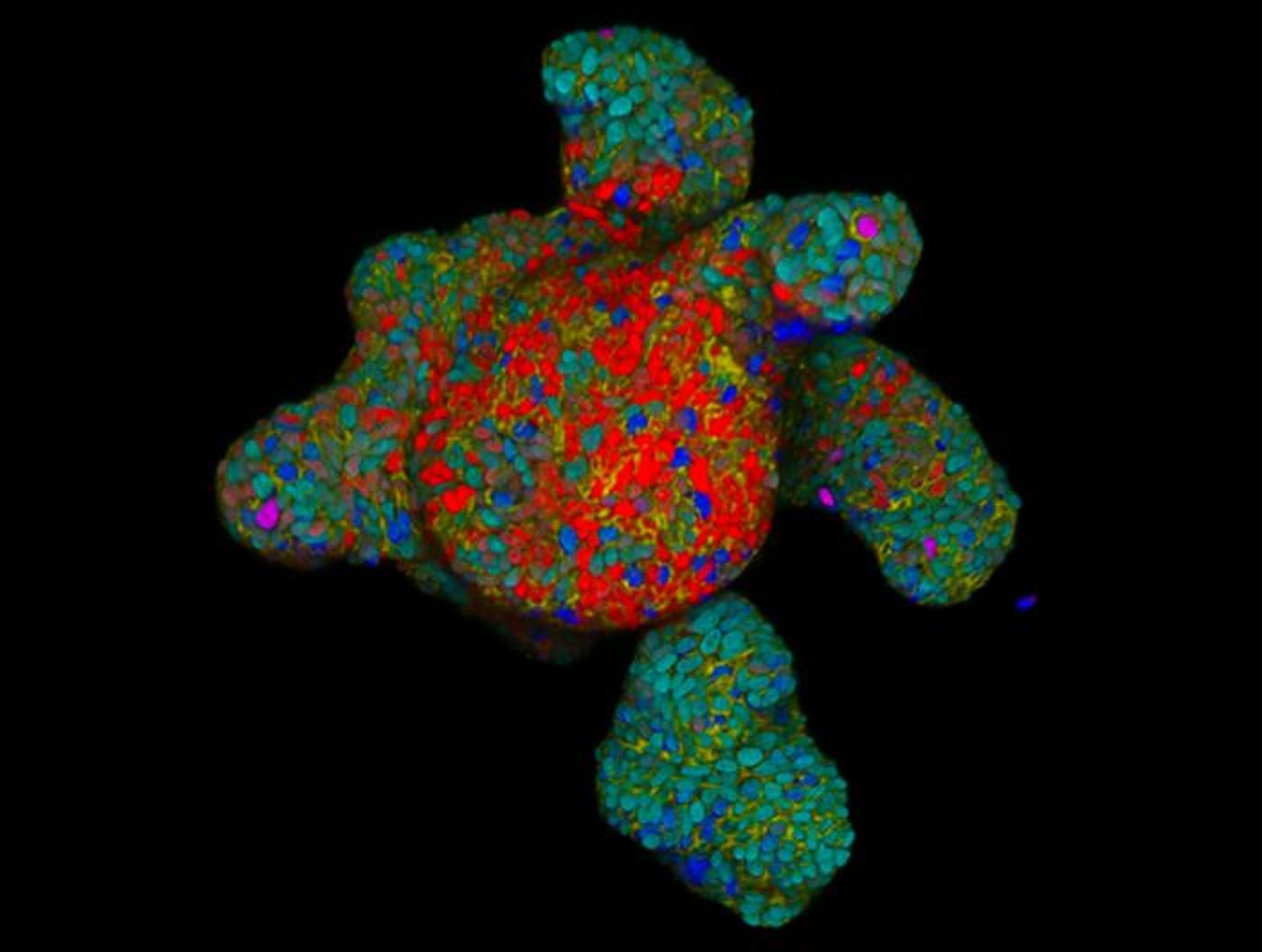
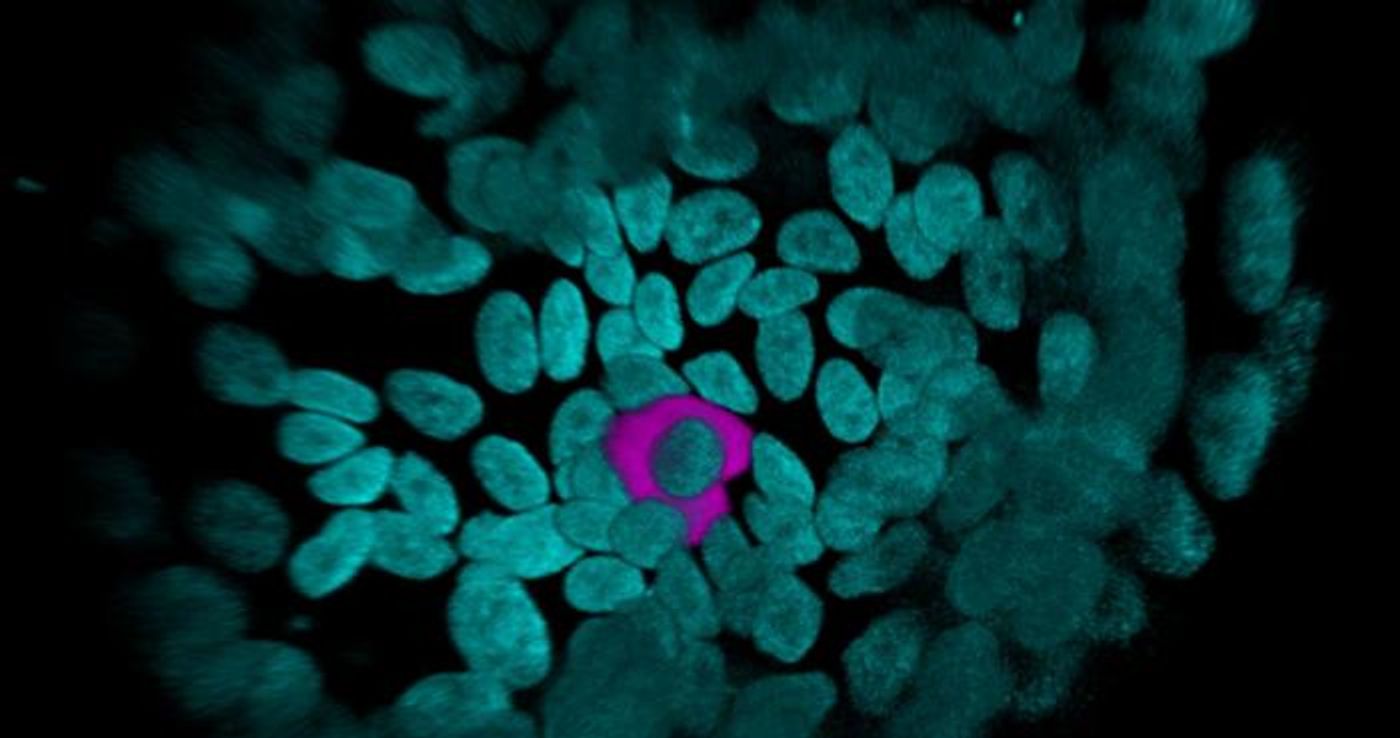
EECs are a relatively rare type of cell, and scientists still don't know a lot about them. In this study, the investigators found a marker on the surface of human EECs called CD200. This marker was then used to collect a large number of EECs from an intestinal organoid model. The scientists then found more molecules that are unique to EECs, including receptors that have not been found in EECs before this. The researchers activated these receptors with different ligands, to reveal receptors that are directly related to the release of hormones from EECs.
The researchers found receptors that could control hormone release in EECs. Then they confirmed these findings with CRISPR, which showed that when certain genes were altered, the release of specific hormones could be blocked.
This study has shown how human EECs react to the activation of specific receptors. This research is a foundation for future studies that may show how certain receptors might be manipulated to treat various disorders such as metabolic or gut motility diseases.
There are already effective medications for metabolic disorders, which are meant to mimic the action of gut hormones, such as GLP-1. But if EECs could be targeted directly to alter hormone levels, it may change therapeutic approaches. Researchers have to understand hormone release in the gut first, and this study is a step in that direction.
Organoids, which are simplified models of the human gut, have provided these insights. The scientists used a protein called neurogenenin-3 to activate the production of higher levels of EECs in their gut organoids. This method led to the release of various hormones, confirming that they work as research models of the human gut.
Sources: Hubrecht University, Science