A Biomarker May Predict the Most Severe COVID-19 Cases
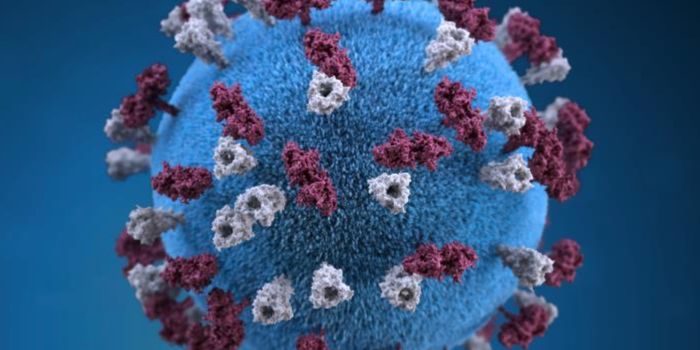
Researchers may have found a way to identify the COVID-19 patients that will need targeted therapies the most. Biomarkers have been discovered that may help clinicians determine who is at risk for having a serious illness from the pandemic virus SARS-CoV-2. The work, which may help doctors save lives, has been reported in Frontiers in Immunology.
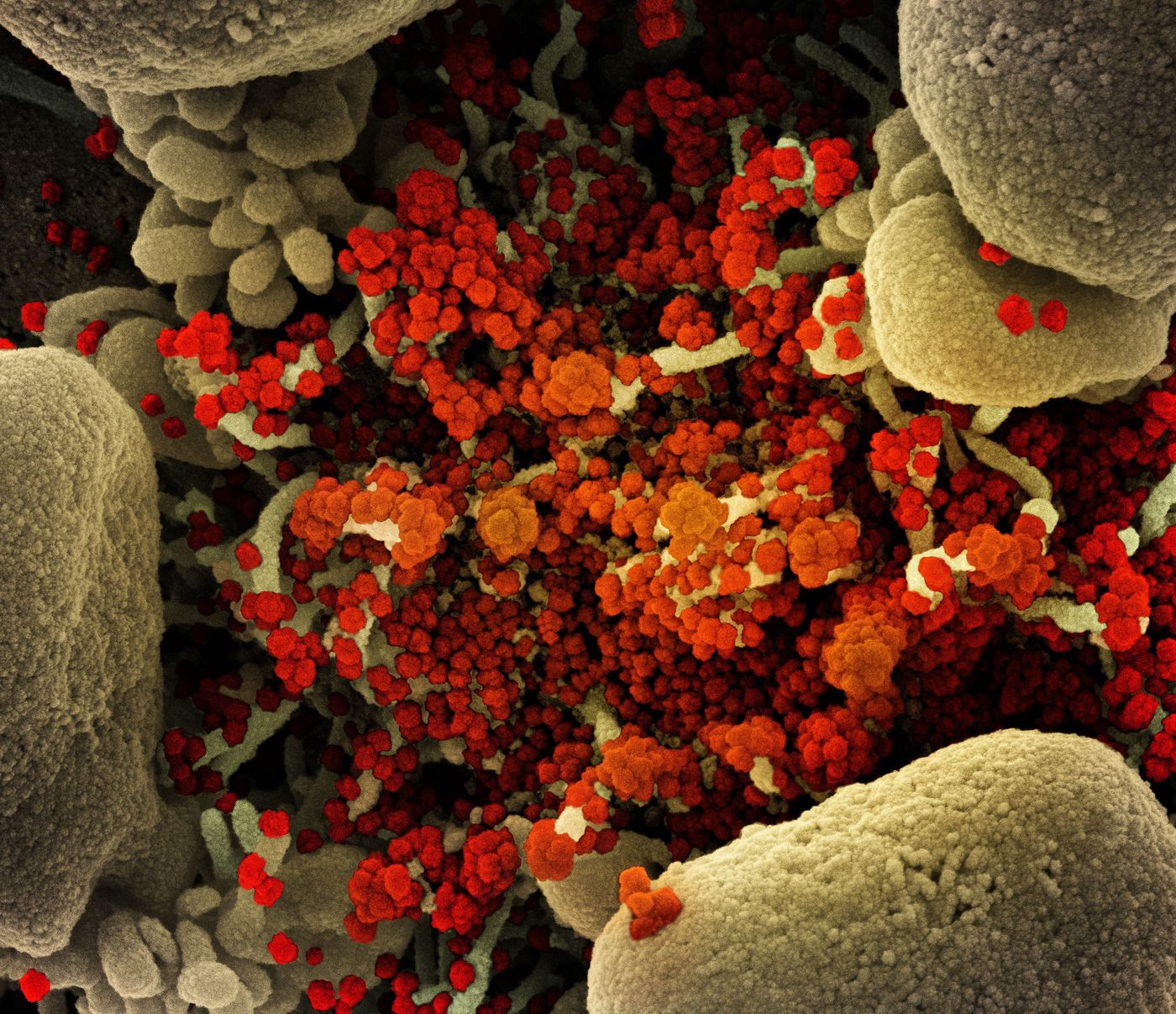
The researchers began by assessing how people's immune systems were responding to SARS-CoV-2 infections, which can range from mild to life-threatening. The immune system has to be very carefully controlled; its response to an invader can overwhelm the body if it's not managed properly. The scientists analyzed RNA sequencing data, which provides a snapshot of the genes that are active in a cell at some given time; in this case, airway cells from healthy individuals and various COVID-19 patients. This publicly available data has been published in previous research by Chinese scientists.
"Our analyses identified an association between immune cells called neutrophils and special cell receptors that bind to the steroid hormone glucocorticoid," explained Professor Heung Kyu Lee of The Korea Advanced Institute of Science and Technology (KAIST). "This finding could be used as a biomarker for predicting disease severity in patients and thus selecting a targeted therapy that can help treat them at an appropriate time," he added.
In some severe COVID-19 cases, an exaggerated immune response has been linked to inflammation that is so excessive it damages the airways. This condition is called acute respiratory distress syndrome (ARDS), and it is responsible for an estimated 70 percent of fatal COVID-19 infections. The mechanisms underlying this problem are not well understood, but it seems to involve an excess of immune cells called neutrophils in the airways.
Lee and KAIST graduate candidate Jang Hyun Park found that immune cells called myeloid cells generate too many molecules like a chemokine called CXCL8 or cytokine called TNF, which recruit neutrophils. Severely ill patients are also not good at recruiting the T cells that have to help attack the virus. Neutrophils themselves can secrete molecules that trap pathogens at normal levels, but cause damage to the airways when the levels are too high.
Increased expression of CXCL8 and excess neutrophil recruitment were also linked to a lack of glucocorticoid receptors.
Glucocorticoids, including dexamethasone, can help stop inflammation. While they may help severely ill COVID-19 patients, if they are used too early or in mild infections, they may suppress the natural immune response to the virus. Glucocorticoid treatment may also be useless for people that already have airway damage.
It will be important to know exactly who benefits from the treatment, like COVID-19 patients with low glucocorticoid receptor expression, high CXCL8 levels, and excess neutrophil recruitment. More work will be needed before these findings can be taken to the clinic, but it can help us learn more about preventing the worst cases of COVID-19.
"Our study could serve as a springboard towards more accurate and reliable COVID-19 treatments," Professor Lee said.
Sources: AAAS/Eurekalert! via The Korea Advanced Institute of Science and Technology, Frontiers in Immunology