Hay Fever? Mind your food!
Spring is almost here and with it comes the return of sunnier days and warmer weather. For some, spring also means the return of itchy eyes and runny noses due to pollen. It is estimated that between 10 and 30 percent of the population worldwide is affected by pollen-triggered hay fever. But did you know those same pollens can also trigger food allergies?
This is known as oral allergy syndrome, OAS, named for the itchy mouth, throat, and ears that occur after eating certain foods. Oral allergy syndrome is usually localized to the mouth and is not life-threatening. In fact, if eating a food results in a reaction that progresses beyond the mouth area, then that food is at risk of triggering the more serious and potentially fatal allergic reaction, anaphylaxis. This type of severe reaction, as well as any reaction following ingestion of legumes (such as peanuts) or tree nuts, should be followed up by consultation with an allergist.
An oral allergy occurs when the immune system, sensitized to pollen, also reacts to fruits and vegetables that have similarly structured proteins. This happens because the pollen-specific immunoglobulin E (IgE) antibody that triggers hay fever recognizes the similar protein structure of the food allergen and triggers an allergic reaction that is localized to the mouth. This cross-reactivity is thought to account for more than 60% of all food allergies in adults, though children are also susceptible. For example, a person allergic to birch pollen may also experience oral allergy symptoms when eating raw apples, apricots, carrots, celery, cherries, kiwis, parsley, peaches, pears, plums, or when eating peanuts, soy beans or tree nuts. In many instances, cooking is enough to denature the food allergen and prevent its recognition by the pollen-specific IgE antibody.
“It has been shown that cooking food can sometimes eliminate allergens in certain species like apples, while it is impossible to destroy allergens in celery and strawberries. For some types of food (e.g., nuts) that contain more than one allergen, heat treatment will destroy certain allergens, but not all.” Journal of Allergy
Thus, the cooked form of the food may be tolerated, but this isn’t foolproof.
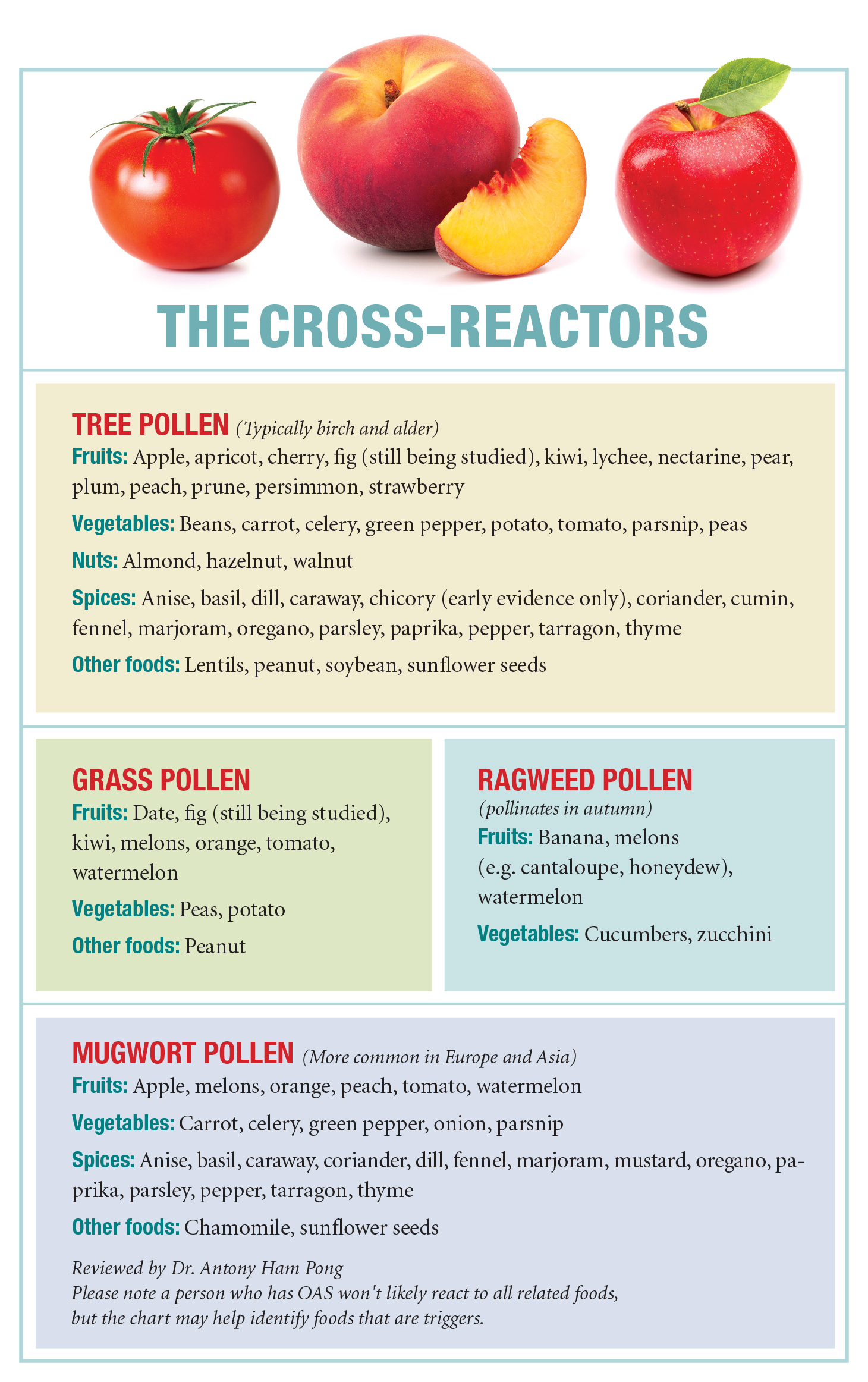
Pollens from birch trees in spring, timothy and orchard grasses in summer, ragweed plants in late summer and mugwort plants in autumn have each been identified as triggers for OAS. Indeed, OAS symptoms may be worse during the season when a specific pollen is present. Still, OAS symptoms can occur at any time regardless of the presence of the pollen. Below is a chart, obtained from Allergic Living Magazine, of foods identified as being cross reactive with pollen.
The best treatment for OAS is avoidance of the offending food. Allergy shots to tolerize against pollen have also shown promise with alleviating OAS symptoms. In the event of an OAS reaction, remain calm. Rinsing the mouth out with water will help remove the allergens causing the reaction and stop the symptoms. If hot, but not boiling water is used, then rinsing may breakdown the allergen causing the reaction to cease within 30 minutes to an hour. If antihistamines are available, it is advised that they be taken but be aware that they may take up to an hour to work. If the reaction involves more that just the mouth, or if the throat begins to swell, then the reaction may be severe and an EpiPen should be used. Speak to a doctor to determine if you’re at risk for a severe allergic reaction and should carry an EpiPen. With the proper precautions and preparations, we’ll all survive until next winter.









