Can Immune cells contribute to Lung Diseases Severity?!
Macrophages are a type of immune cell that can detect and destruct bacteria, viruses, and harmful materials. They are an essential part of lung immunity; however, sometimes they can contribute to the development and severity of some lung diseases.
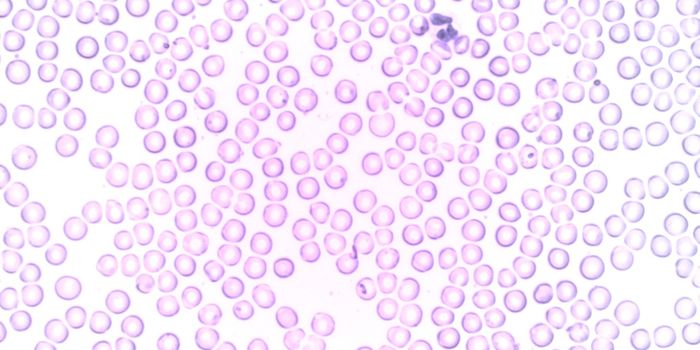
Macrophages can either develop from embryonic precursors or from blood monocytes that develop from hematopoietic stem cells, " stem cells that give rise to blood cells" in the bone marrow. Monocytes are classified into main types; in humans, two are classical CD14+ monocytes and non-classical CD16+ monocytes.
It is then important to study human macrophage development to try to identify which types of macrophages contribute to the development of lung diseases. Still, it is challenging to study human macrophages in vivo "in cells," and little research has been done on their development until a group of researchers from Karolinska Institutet in Sweden developed a humanized mouse model to study human macrophage's developmental stages from blood monocytes.
"Certain macrophages in the lungs probably have a connection to a number of severe lung diseases. In respiratory infections, for example, monocytes in the lungs develop into macrophages, which combat viruses and bacteria. But a certain type of macrophage may also contribute to severe inflammation and infections," says the study's first author Elza Evren, a doctoral student in Tim Willinger's research team.
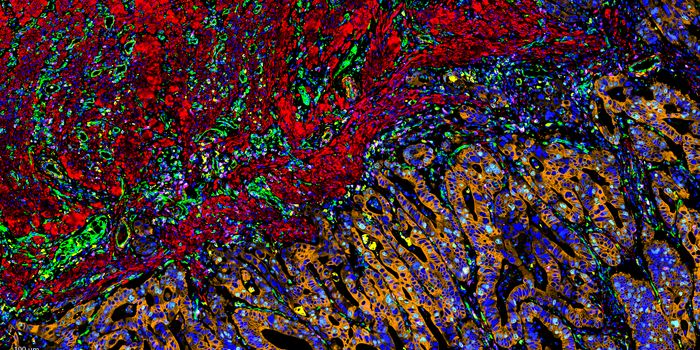
To resemble the microenvironment surrounding human macrophages for accurate study, the humanized mouse model was transplanted with hematopoietic stem cells, and genetically modified to express factors that are important for human blood cells and macrophage development.
It was revealed that blood classical CD14+ monocytes migrate into the lung tissues and develop alveolar macrophages, interstitial macrophages " that are present between the lung's epithelial tissues and the blood vessels surrounding it" and lung monocytes, while non-classical CD16+ monocytes develop into pulmonary intravascular macrophages.
The study that was published in Immunity also identified a special monocyte, HLA-DRhi, an intermediate between blood monocyte and lung macrophage.
Researchers believe that in COVID-19 infection, the protective anti-inflammatory macrophages are replaced with pro-inflammatory monocyte-derived macrophages since other studies showed that the presence of blood monocytes-derived macrophages correlates with the severity of COVID-19 disease and the extent of lung damage.
Also, it was found that severely ill COVID-19 patients have fewer HLA-DRhi monocytes in their blood, which could mean their migration into the lungs.
These findings show that blood monocyte-derived macrophages might have a role in inflammatory responses, which leads the researchers to recommend that future treatments should focus on those macrophages and monocytes for either lung disease prevention or reducing COVID-19 infection severity.
Watch the video below to learn about macrophage function.
Sources: Medical Xpress via Karolinska Institutet