Genes That Destabilize Cells Increase Risk of Diabetes
In the United States, over 10% of the population has diabetes. Roughly 1 million individuals each year are diagnosed. As a result, over 25 million people nationwide have diabetes and seek medical treatment. There are two subcategories of diabetes, type 1 and type 2, which relate to how diabetes occurs. Type 2 diabetes is the most common and accounts for about 90% of the diagnosed population. The cause of type 2 diabetes is when the pancreas generates less insulin than required and the body becomes resistant. Specific symptoms include thirst, fatigue, blurry vision, hunger, and irritability, among others. Unfortunately, there is no cure for diabetes, and scientists are still working to improve treatments. However, another limited aspect of diabetic research addresses the impact of insulin resistance on cell metabolism.
Cells in the pancreas and the rest of your body can handle stress to a point. After enough burden, cells break down and cause dysfunction throughout the body. Stress, including inflammation and high blood sugar, can cause pancreatic cells to break down and cause an individual to develop type 2 diabetes. A significant research topic within the field of diabetes includes investigating this stress on cell metabolism.
A recent article in Cell Metabolism by Drs. Duygu Ucar, Michael Stitzel, and others demonstrated that the risk of diabetes is dependent on how well an individual’s pancreatic cells can handle stress. Drs. Ucar and Stitzel are both professors at the Jackson Laboratory in Farmington, Connecticut. Their research investigates gene expression levels in different disease states. Dr. Stitzel focuses explicitly on diabetes and the regulatory mechanisms within cells that dictate function and activity.
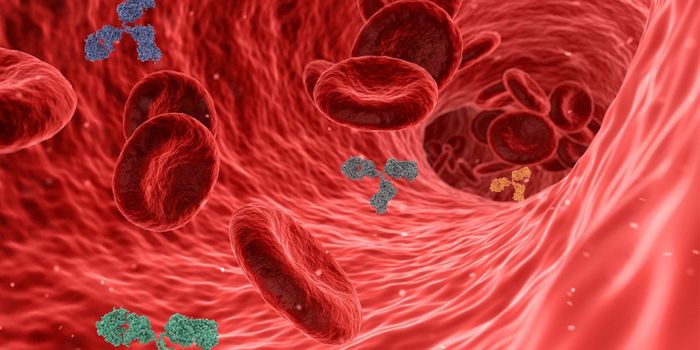
The team found that specific gene expressions make cells less likely to handle stress, including inflammation. As a result, the cells die, and the patient is at a higher risk of developing type 2 diabetes. To overcome this risk, researchers identified different gene expression patterns that relate to cell stress and diabetes. Previous work has shown that mitochondrial and protein stress leads to slower function and death in pancreatic cells that produce insulin, known as islet beta cells. Ucar, Stitzel, and the team used various laboratory techniques and next-generation sequencing to identify gene expression and how these genes were regulated to determine which cells influenced this slower function and death after prolonged exposure to stress.
Cells contain packed DNA in the nucleus until it is time to replicate or respond to outside stimuli. Certain areas of the DNA are loosely unpacked, allowing the cells to upregulate genes that code for protein synthesis and function outcomes. Researchers exposed cells to stress and tracked intracellular changes to take advantage of this process. They then recorded how gene expression was regulated based on loosely packed DNA regions. They found that over 5,000 genes in the islet cells were changed, and many were involved in protein production. The team concluded that patients with identified genetic variants are more at risk for diabetes.
Ucar, Stitizel, and others hope this work will translate to the clinic and better inform physicians of their patient's risk factors. For example, a gene named MAP3K5, which plays a critical role in islet cell death, was upregulated in response to mitochondrial death. However, by blocking this gene, the cells became resistant to stress and did not die. Researchers hope this can be a targetable gene for patients and reduce their risk of diabetes as a preventative medical approach.
Article, Cell Metabolism, Duygu Ucar, Michael Stitzel, Jackson Laboratory