Gene Regulation Improves Immune Cell Therapy
New therapeutic approaches are on the horizon, offering hope for the treatment of various diseases, including solid tumors. Previous cancer therapies, such as chemotherapy and surgery, were limited to the time of diagnosis and often had off-target effects, making the therapy toxic to patients. However, novel approaches to treating cancer have emerged in the last few decades, showing promising clinical success rates when combined with standard-of-care. Immunotherapy, in particular, has revolutionized the way oncologists treat patients, focusing on immune cells to recognize and target the tumor. This unique approach, unlike the standard of care, redirects the body’s cells to prevent tumor proliferation and spread.
Many immunotherapy treatments, with a primary focus on T cells, are a result of collaborative efforts. T cells, responsible for lysing or killing tumors, are regulated by other cells, making the enhancement of T cell function a major research interest. Scientists from various fields are currently working together to improve immunotherapy through combination treatments and cellular engineering.
Recently, an article in Science by Dr. Caitlin C. Zebley and others demonstrated that blocking a specific gene, known as Asxl1, improves T cell function and enhances a traditional immunotherapeutic strategy. Zebley is a physician-scientist and Assistant Professor in the Department of Bone Marrow Transplantation & Cellular Therapy Comprehensive Cancer Center at St. Jude Children’s Research Hospital. Her research focuses on the fundamental mechanisms of T cell biology. Specifically, her work has investigated improving T cell therapy in solid and hematologic malignancies.
The immunotherapy Zebley and others focus on improving is known as immune checkpoint inhibitors (ICI). Immune cells, specifically T cells, express markers or checkpoints on their surface, which prevent the T cell from activating and targeting tumors when bound to a ligand on corresponding cells. In the last few decades, research has shown that blocking this T cell marker allows the T cell to activate and recognize malignant cells. However, this therapy as a single agent is less efficacious than combination therapies. Therefore, researchers, including Zebley, are finding new ways to improve ICI.
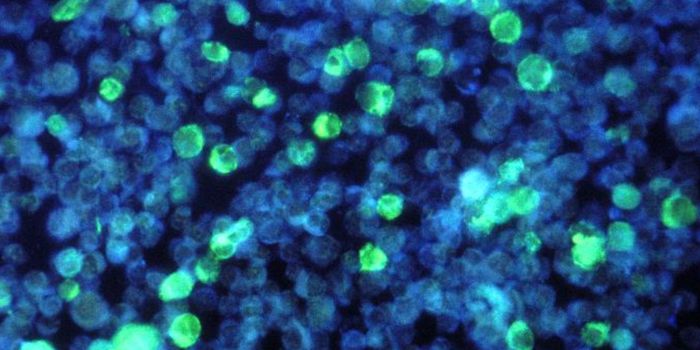
Zebley and others used animal models and next-generation sequencing techniques to discover how Asxl1 dysregulation enhances ICI. Interestingly, they took mice without the Asxl1 gene and found that they responded better to ICI than intact Asxl1. The group without Asxl1 had improved effector and antitumor function. Therefore, it was concluded that Asxl1 controls T cell differentiation in which the cells mature and develop into an “exhausted” state where the cells cannot become activated and execute their function. Researchers propose that this discovery can develop T cell therapy and engineer cells to perform better. The group first suspected the involvement of this gene when analyzing cells from patients who were successfully treated with ICIs. These patients were found to have mutated Asxl1 in their T cells, allowing successful ICI treatment.
Zebley and others, for the first time, discovered this gene as a critical marker in T cell development and its implications in cell therapy. This work provides foundational knowledge about the function of T cells and how healthcare professionals can overcome T cell exhaustion through gene regulation. Overall, this discovery has the potential to enhance ICI therapy in the clinic and improve patient outcomes and quality of life.
Article, Science, Caitlin C. Zebley, St. Jude Children’s Research Hospital