Gut Microbes Play a Role in Neurodegeneration
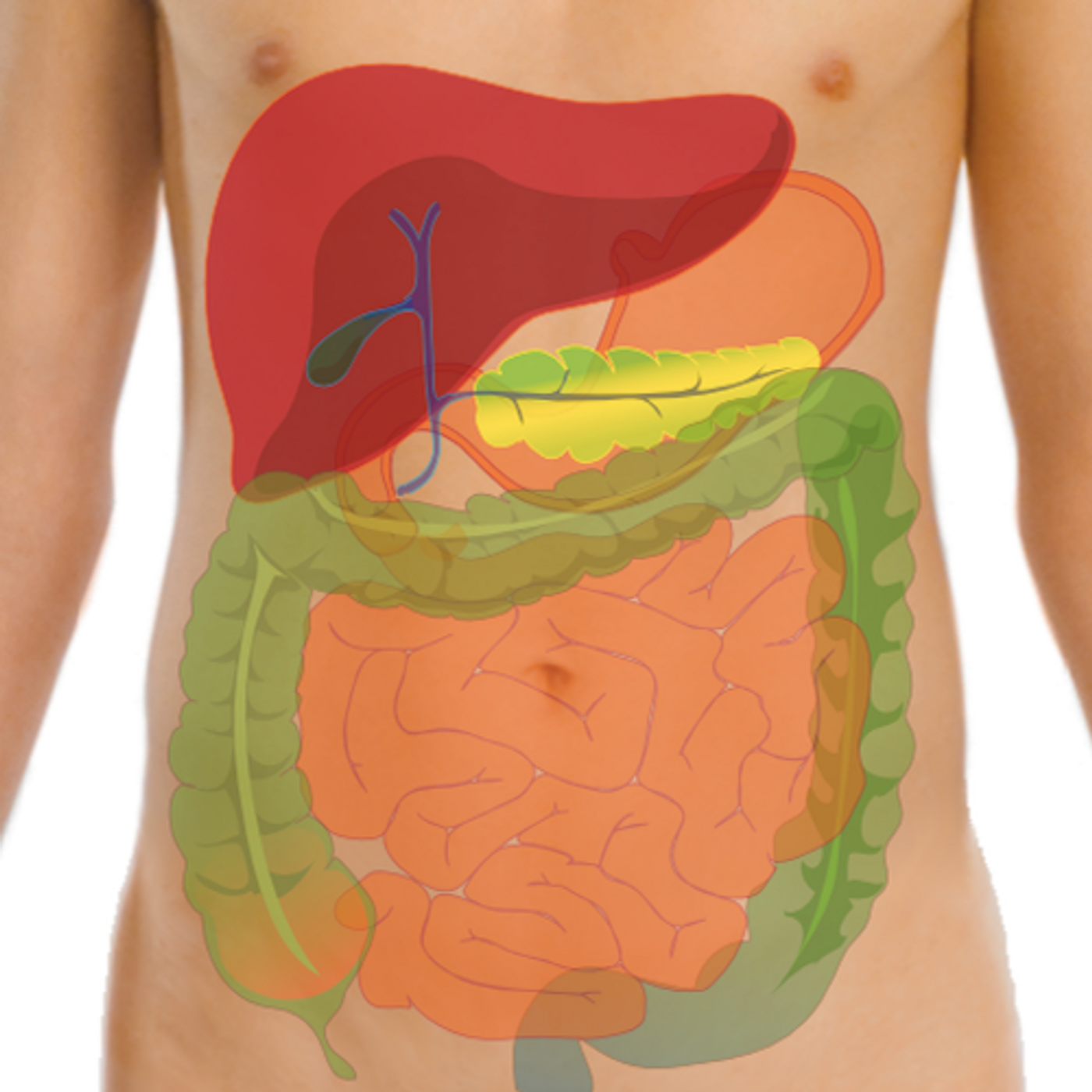
Humans host communities of microbes in and on our bodies; the microorganisms that reside in our gut have been shown to have a significant influence on our health and well-being. That community, our gut microbiome, has been shown to play a role in metabolism and immunity. Recent research has also connected it to the neurodegenerative conditions Parkinson's and Alzheimer's diseases; it may play a role in the progression and even cause of those disorders. Now, work by University of Louisville neurology professor Robert P. Friedland, M.D., and Matthew R. Chapman, Ph.D., a professor at the University of Michigan suggested that a new term should be used to describe the interaction between the gut microbiome and the brain: mapranosis.
The term "mapranosis" is defined in the new PLOS Pathogens publication; it refers to the process by which microbially-produced amyloids change protein structure and promote nervous system inflammation. Those structural alterations, proteopathy, augments or initiates disease in the brain. The term comes from Microbiota Associated Protepathy And Neuroinflammation + osis. Friedland is hopeful that by naming the process, awareness and research in the area will broaden.
"It is critical to define the ways in which gut bacteria and other organisms interact with the host to create disease, as there are many ways in which the microbiota may be altered to influence health," noted Friedland.
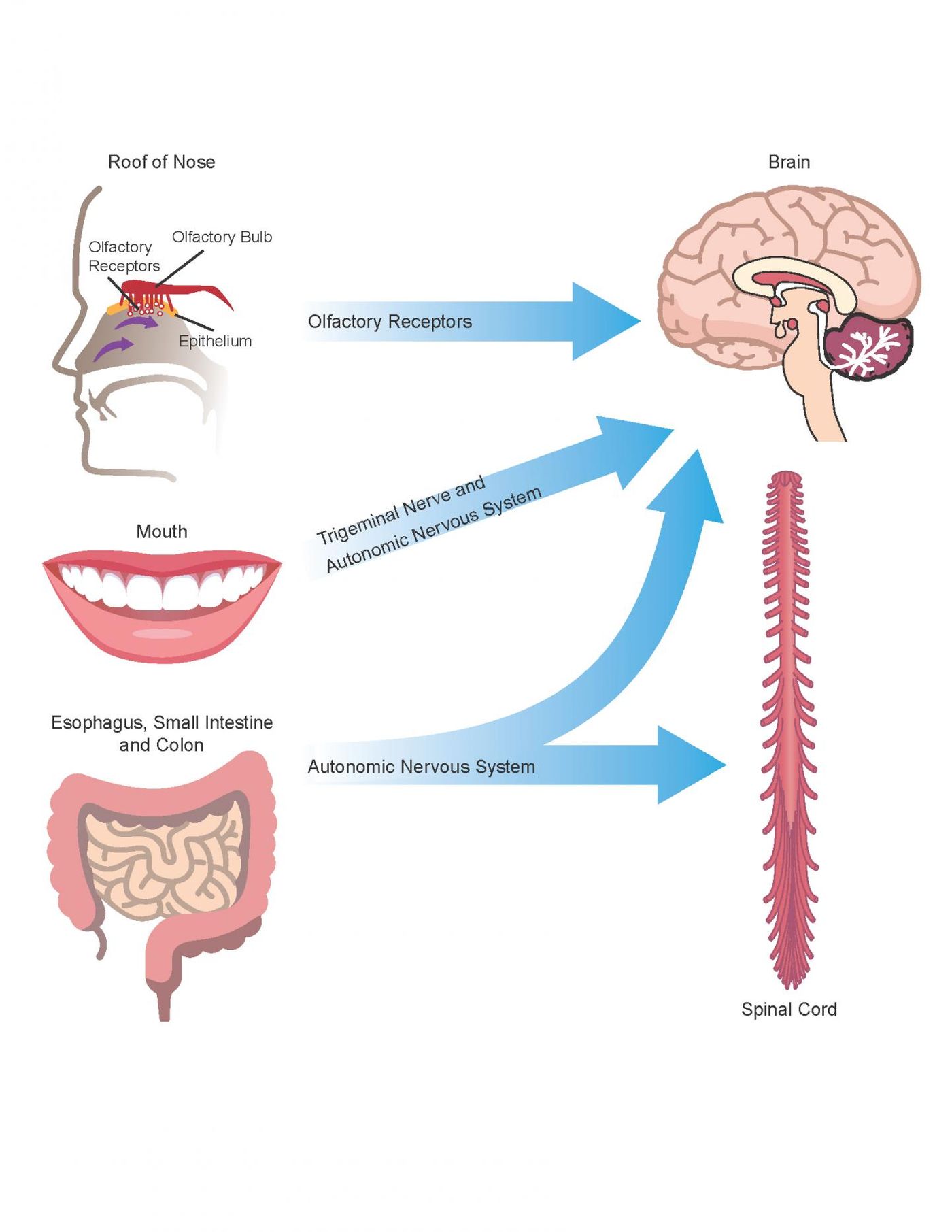
When genomics tools got more powerful, it became much easier to assess microbial populations in the gut, expanding the field of study rapidly. While the work continues, it has also been established that the gut is directly connected to the brain, and the gut microbiome influences the brain in a relationship called the gut-brain axis.
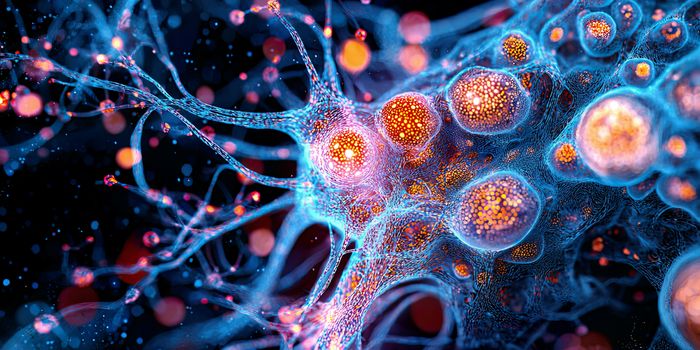
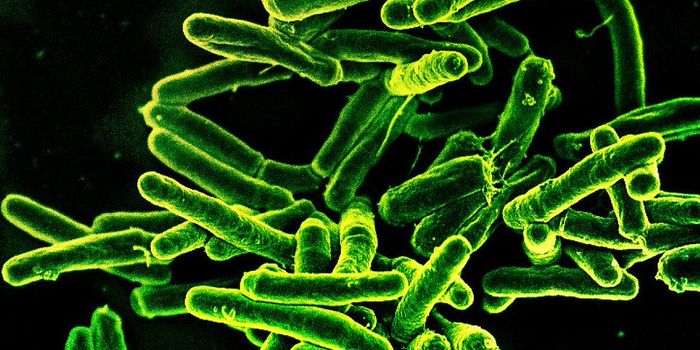
Research has linked neurodegeneration to misfolded amyloid proteins clumping up in the brain. "It is well known that patterns of amyloid misfolding of neuronal proteins are involved in age-related brain diseases. Recent studies suggest that similar protein structures produced by gut bacteria, referred to as bacterial amyloid, may be involved in the initiation of neurodegenerative processes in the brain," Friedland explained. "Bacterial amyloids are produced by a wide range of microbes that inhabit the GI tract, including the mouth."
Previous work by Friedland and colleagues indicated that gut bacteria, Escherichia coli, in rodents and worms created misfolded amyloid proteins. Intriguingly, the amyloids found in the brains of those models also misfolded; that phenomenon is called cross-seeding.
"Our work suggests that our commensal microbial partners make functional extracellular amyloid proteins, which interact with host proteins through cross-seeding of amyloid misfolding and trigger neuroinflammation in the brain," Friedland suggested.
This work also explored other factors that connect microbiota and neurodegeneration. The microbiome alters immune processes in the body, as well as in the nervous system. Because gut bacteria may increase oxidative toxicity, it may increase the inflammation that can contribute to neurodegeneration. Additional research in this area may help reveal new therapeutic options for neurodegeneration.
Sources: AAAS/Eurekalert! Via University of Louisville, PLOS Pathogens