Anti-Epileptic Stem Cells
Epilepsy, a fourth most common neurological disease is estimated to develop during the lifetime of approximately, one in every twenty-six people in the United States. Together with its comorbidities depression and anxiety it significantly affects the quality of life. Despite successful pharmacological treatments, around 30-40% of them continue to have seizures and opt for invasive surgical therapies.
Temporal lobe epilepsy (TLE) exhibits characteristic spontaneous recurrent seizures (SRS) is often caused post hippocampal injury. The conventional antiepileptic drugs offer limited remission and alternative treatment strategies like patient-specific cell therapy gained a lot of interest. Gamma-Aminobutyric acid (GABA) interneurons are the critical players in TLE pathology, and loss of these neurons halts the inhibitory neurotransmission and leads to seizures.
Researchers from the Texas A&M College of Medicine, demonstrated that grafting of medial ganglionic eminence (MGE)-derived GABA-ergic progenitor cells into the hippocampus subdued the seizures and alleviated resultant cognitive, memory and mood dysfunctions associated with prolonged TLE. Further, silencing of the graft-derived GABA interneurons suppressed the antiepileptic effects confirming the inhibitory effect induced by them when active.
The research team was led by Ashok K. Shetty, Ph.D., a professor in the Department of Molecular and Cellular Medicine at the Texas A&M College of Medicine, associate director of the Institute for Regenerative Medicine and a research career scientist at the Olin E. Teague Veterans' Medical Center, part of the Central Texas Veterans Health Care System. Together, they are working on better and permanent treatment for epilepsy. Current study results were published last week in the Proceedings of the National Academy of Sciences (PNAS).
"What we did is transplant human induced pluripotent stem cell-derived GABAergic progenitor cells into the hippocampus in an animal model of early temporal lobe epilepsy," Shetty said. The hippocampus is a region in the brain where seizures originate in temporal lobe epilepsy, which is also important for learning, memory, and mood. "It worked very well to suppress seizures and even to improve cognitive and mood function in the chronic phase of epilepsy."
Further testing showed that these transplanted human neurons formed synapses, or connections, with the host excitatory neurons. "They were also positive for GABA and other markers of specialized subclasses of inhibitory interneurons, which was the goal," Shetty said. "Another fascinating aspect of this study is that transplanted human GABAergic neurons were found to be directly involved in controlling seizures, as silencing the transplanted GABAergic neurons resulted in an increased number of seizures."
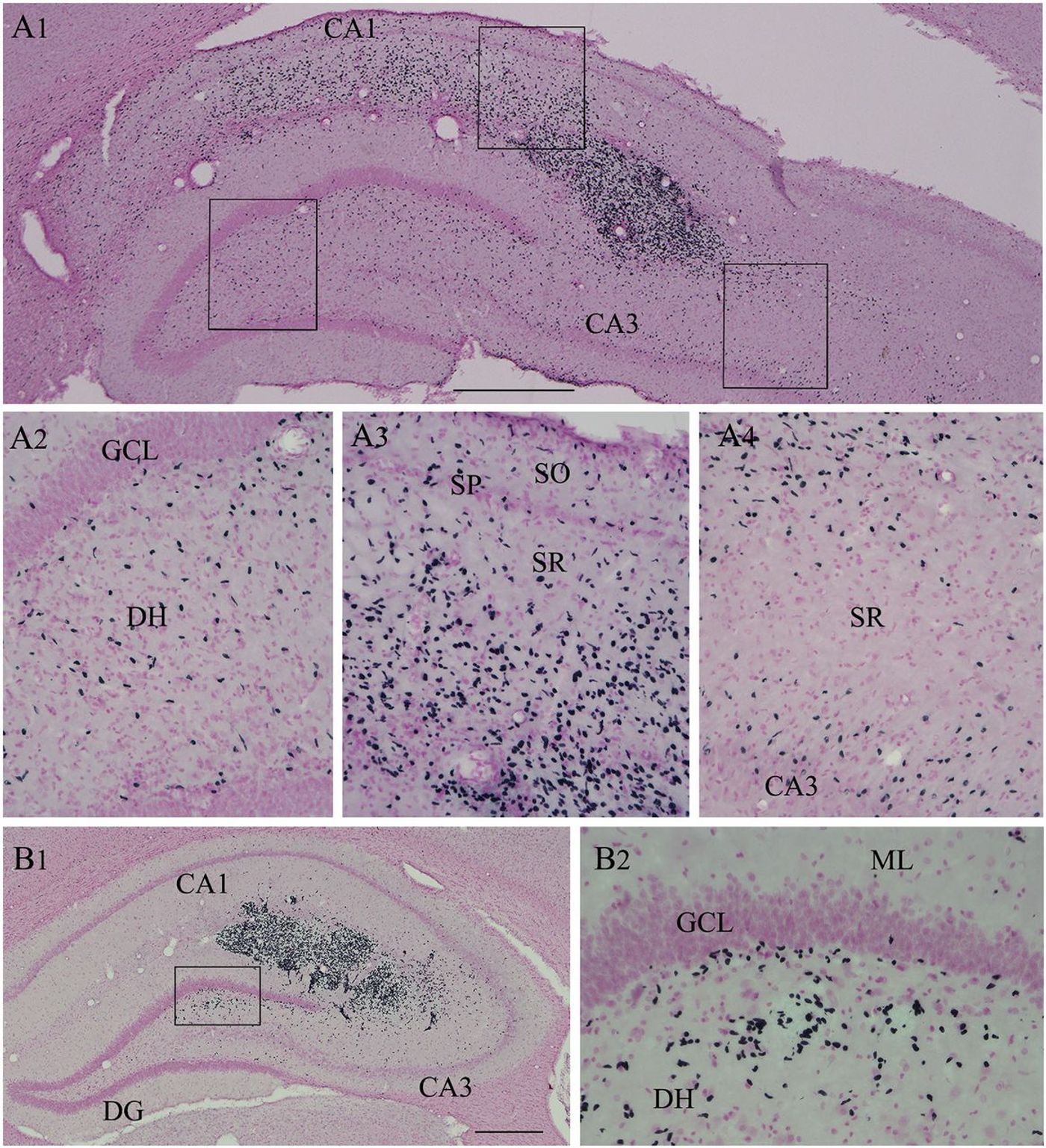
Cells derived from hMGE-like cell grafts placed into the hippocampus after SE pervasively migrated to different subfields and layers of the hippocampus.Image Source: Upadhya et al., PNAS
"This publication by Dr. Shetty and his colleagues is a major step forward in treating otherwise incurable diseases of the brain," said Darwin J. Prockop, MD, Ph.D., the Stearman Chair in Genomic Medicine, director of the Texas A&M Institute for Regenerative Medicine and professor at the Texas A&M College of Medicine. "One important aspect of the work is that the same cells can be obtained from a patient." This type of process, called autologous transplant, is patient-specific, meaning that there would be no risk of rejection of the new neurons, and the person wouldn't need anti-rejection medication.
"We will need to make sure that we're doing more good than harm," Shetty said. "Going forward, we need to make sure that all of the cells transplanted have turned into neurons because putting undifferentiated pluripotent stem cells into the body could lead to tumors and other problems."
"A great deal of research is required before patients can be safely treated," Prockop said. "But this publication shows a way in which patients can someday be treated with their cells for the devastating effects of epilepsy but perhaps also other diseases such as Parkinsonism and Alzheimer's disease."
The author's advice not to generalize this treatment strategy yet, as the current study targets specifically the hippocampal injury induced by status epilepticus and cell therapy is early intervention. Although suggested to take these findings with a grain of salt, translating the therapeutic effects to other forms of epilepsy, particularly drug-resistant epilepsy is the logical next step. "Currently, there is no effective treatment for drug-resistant epilepsy accompanying with depression, memory problems, and a death rate five to 10 times that of the general population," Shetty said. "Our results suggest that induced pluripotent stem cell-derived GABAergic cell therapy has the promise for providing a long-lasting seizure control and relieving co-morbidities associated with epilepsy."
Questions to ponder over about stem cell therapy, a) differentiation efficiency of the grafted stem cells to GABA-ergic interneurons and b) Tumor formation. The work reports 76% differentiation efficiency; but is it enough? Also, to avoid the potential tumor formation, the authors suggest using purified, postmitotic cells, which warrants more work.
Watch the video to learn about epilepsy treatment with stem cell therapy and advances in neurological Stem Cell Therapeutics.
Sources: Texas A&M College of Medicine, Proceedings of the National Academy of Sciences (PNAS).